Anytime is a great time to set goals and become the best version of yourself. Now, in the age of COVID-19, it may be an even better time. While not conclusive, several studies suggest smokers who develop COVID-19 are up to 14 times more likely to need intensive treatment. For many, this is just the motivation needed to tackle tobacco habits once and for all.
When you’re a tobacco user, whether it be smoking cigarettes, a cigar, a pipe, or chewing tobacco, it is not just a physical addiction but also a mental addiction. Often it feels like a way to cope with the stress of life’s challenges. So, trying to quit is more than just vowing to put the cigarette down or spit out the chew, it can challenge your entire being.
“One of the first things we explore are the reasons for quitting,” said Aaron Korte, RN, RCEP, CDE, CTTS, who coordinates the Welia Health tobacco cessation program.
“People are often surprised at their reasons for quitting. We talk about the obvious; financial, family, and health. Then as we talk longer, people realize they want to quit for a grandchild or child, or that cigarettes make everything smell bad. The person often explains how cigarettes or chewing tobacco has changed how they interact with their family and friends. They are just plain tired of being controlled by the addiction,” said Aaron.
Aaron Korte, RN, RCEP, CDE, CTTS
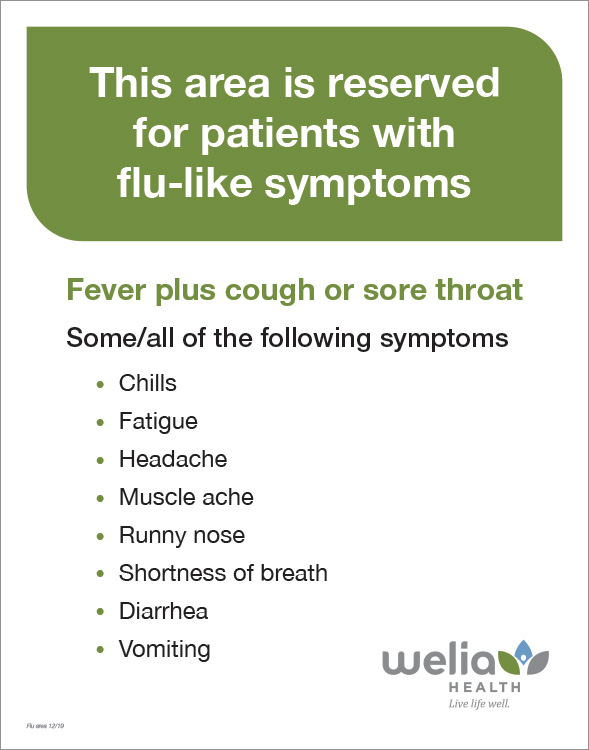
Welia Health’s tobacco cessation program
When you’re ready to quit, the Welia Health team is here to help. The program is covered by most insurance plans and others may qualify for reduced or free sessions if coverage is not available.
On average, Aaron meets with folks 3 to 4 times or more, if needed. The first appointment generally takes 45 minutes to review all available options to help people succeed. “I’ve found that the best tobacco cessation plan is one that the person comes up with…and I’m here to support it with the medical and emotional approaches that are available,” said Aaron. Before leaving the first visit, people will have an individualized plan for quitting.
There are several methods for quitting tobacco: nicotine replacement options, prescribed medications, or other holistic choices. Most opt for a combination of them all.
Tools for quitting
- Nicotine Replacement: Nicotine is an addictive drug in tobacco products. With nicotine replacement, patients use patches, gum or lozenges, all sold over-the-counter to help curb the craving. Another replacement option is used as either an inhaler or a nasal spray. Aaron will work with your provider to get the required prescription. Whichever delivery mechanism is chosen, the core concept is the same, to replace the nicotine while using a “clean” delivery option versus cigarettes or chewing tobacco which utilizes a carcinogen as the delivery method.
- Other prescription options: There are other prescriptions available to help decrease the person’s need or want for nicotine. Most people can kick their tobacco habit using a prescribed medication in about 2 to 3 weeks, but on the flip side, due to some side effects, it doesn’t work for everyone.
Between your provider’s guidance and the support of the tobacco cessation program support, you will find the best medication to fit your individualized plan.
Holistic options to explore
- Hypnosis: Hypnosis can work by weakening the desire to quit or strengthening the person’s will to discontinue use. It’s not the state of clucking like a chicken, rather it’s a teacher (the hypnotist) helping you, to convince yourself to do something you are most capable of doing. There is not a ton of evidence showing the effectiveness of this treatment yet is still an option for those willing to try.
- Acupuncture: With many local businesses providing acupuncture, this is another safe way to help reduce nicotine cravings and other discomforts. Acupuncture uses needles and body-specific points to entice the brain to release endorphins, our feel-good hormones that cope with the effects of withdrawal associated with quitting tobacco. As with all choices, this can work for some but maybe not for all.
Considerations when quitting tobacco
In addition to the issues around one’s personal identity, consider these factors.
- Quitting can take practice: Most people need to practice learning how to not smoke or chew just as they learned to use their tobacco of choice. “When that person comes back for a follow-up visit and says they are not a smoker (chewer) and they have been feeling the health rewards (better breathing, less smell, less coughing, more money in their bank account) that is very exciting to be a part of!” says Aaron.
- Weight gain: Food and physical activity are also addressed during the visits. If able, increasing physical activity is important to ward off weight gain. Some people decide to join a fitness center with the money saved from not smoking, others try to work in more activity on a daily basis. Discussing food choices is often very helpful. Helping to choose better snack and meal options can eliminate or decrease the weight gain that can sometimes accompany quitting tobacco.
- Societal considerations: Many people feel pressure to smoke when they’re in a social situation where they used to smoke or use. Aaron recommends that people might want to take a break from these, at least for a while. He often gives guidance on what to do in social situations where using tobacco is a trigger. Or if alcohol is a cue, Aaron recommends changing the type of drink you typically consume, like swapping a beer for a fruity drink to reduce cravings.
- And lastly, plain old accountability: People who are trying to quit typically are more successful when they are dedicated to following through and committing to the instructions of their quit plan.
Call 320.225.3356 to schedule an appointment and get on the road to becoming a former tobacco user.