It’s quite possible the birth control you chose five years ago, or even one year ago may no longer be the one that makes the most sense for you. With so many birth control options on the market today, having accurate, up-to-date information is the first step in deciding which is the best choice for you and your specific circumstances. Your Welia Health providers have outlined popular options for birth control.
Remember not all options provide protection against sexually transmitted diseases, and we advise you to speak with your healthcare provider about that.
Abstinence
In its simplest form, abstinence is the decision not to have sexual intercourse. However, it does mean different things to different people. Some people might view abstinence as refraining from all sexual activity. Others might engage in outercourse, avoiding penetration. Used as a form of birth control, when abstinence is followed 100% of the time, it is 100% effective.
Non-hormonal birth control
Short-term, impermanent options
Condoms
If you’re looking for an inexpensive, convenient form of birth control that doesn’t involve a trip to the doctor’s office, then condoms might be an option for you. Condoms are approximately 87-90% effective when used properly. When purchasing condoms, pay particular attention to the size to ensure a proper fit. A couple of things to keep in mind when using condoms, be mindful of long fingernails and jewelry as to not rip or break the latex, and upon withdrawal, hold the condom in place. One common complaint to be aware of is the decreased sensitivity for both males and females.

Female condoms
In 1993, the female condom was approved by the FDA and yields an 85% effective rate when used properly. Female condoms can be purchased over-the-counter (OTC) like male condoms, however, typically cost more. Disadvantages include unpleasant noises, lack of lubrication, and difficulty inserting.

Spermicide
Spermicide is a contraceptive substance that immobilizes or kills sperm before they enter the uterus. The very first spermicide dates back as far as 1850. Today, spermicide can be found in creams, films, foams, gels, and suppositories. They must be used before sexual activity and are 70-90% effective. Effectiveness rates vary based on the quantity of spermicide used, how well the package directions were followed, and timing prior to sexual intercourse. When used with an additional barrier method (condom–male and female, diaphragm, cervical cap, or contraceptive sponge), effectiveness may increase slightly.
New to the market is a vaginal pH regulator gel (Phexxi) that immobilizes sperm so they cannot fertilize an egg. Phexxi is available by prescription only.
Spermicides are easily accessible, inexpensive, offer additional lubrication during sexual activity, and do not contain hormones. However, if you are a high risk for contracting HIV or have HIV/AIDS, get frequent urinary tract infections, are younger than 30 and have sex three or more times a week, you may wish to choose another type of birth control. Things to consider—you and your partner may experience itching, burning or general irritation. In addition, spermicides can be messy and reduce spontaneity as spermicides need to be in place 15 minutes prior to penetration.
Diaphragms and cervical caps
Two other non-hormonal barrier methods include the diaphragm and cervical cap. Both are cup-like devices that securely fit over the cervix to block sperm from entering the uterus. Both require an annual visit with a healthcare provider for proper fitting as well as instruction on techniques for insertion and removal. Because of the variety and availability of other contraceptive methods, these have fallen out of favor and are increasingly more difficult to obtain supply for.

Natural family planning (NFP) / cycle planning
Sometimes referred to as fertility awareness, natural family planning (NFP) is a contraception method where the woman carefully predicts and records her fertile and infertile days as cues about when to avoid sex.
This method of birth control yields an effective rate of about 76% when a woman’s body temperature, calendar, and mucus secretions are carefully tracked. Benefits of NFP include no medications, doctor visits (after the initial consultation to learn about NFP) and can provide increased knowledge of the women’s reproduction cycle.
Hormonal birth control
Oral contraceptive, “the Pill”
In 1960, the FDA approved the sale of the first oral contraceptive. “The Pill,” which is synthetic progesterone and estrogen, stifles the monthly ovulation process. When taken correctly and consistently, it is 98-99% effective in preventing pregnancy.
Side effects are minimal, with most women experiencing them within the first three months. Menses tend to be lighter, more regular and many experience less cramping. Other side effects can include breast tenderness, headaches, nausea, and irregular bleeding. Some women also experienced changes in their sex drive.
The pill is available by prescription only and is covered by most insurance plans. In addition, some reduced or low-cost women’s clinics offer this method of birth control at no cost.
Keep in mind that there is an increased risk for blood clots, heart attacks, stroke, and increased blood pressure for some women and for those over the age of 35 or who use tobacco appear to be at greater risk for severe side effects.
The Minipill, a progesterone-only version of the pill, is safe to use while breastfeeding, however, is not as effective as the regular “pill” which contains both progesterone and estrogen.
“The patch”
A small thin bandage-like sticker adheres to the buttocks, arm, abdomen, or upper torso. It is easy to use and works similar to the pill. Effectiveness is excellent with typical use. The patch should be changed 3 times a month (weekly) and then left off for one week to allow for menses. A combination of estrogen and progesterone prevents the ovaries from releasing an egg.
Side effects are minimal, including lighter, regular and shorter menses, spotting, mood changes, nausea and breast tenderness. Some women have experienced skin reactions to the adhesive.
For those interested in becoming pregnant, after you stop using the patch, you can generally get pregnant within 1 to 2 weeks.

Vaginal ring, brand name NuvaRing®
The NuvaRing® is a small, flexible circular piece of plastic, very similar to a rubber band hair tie, that has a high effectiveness rate when used correctly. This option works much like the pill and patch, containing a combination of estrogen and progesterone that prevent the ovaries from releasing an egg.

NuvaRing is easily inserted into the vagina, similar to how a tampon is inserted. The medication is absorbed through the vaginal walls and remains in place for three weeks and is then removed and discarded on the fourth week to allow menses.
Minor side effects have been reported, mainly annoyances, including some discomfort while the body gets used to the hormonal changes: breast tenderness, nausea, and spotting. Like the pill and the patch, NuvaRing releases hormones that can lead to blood clots. If you have a history of blood-clotting, NuvaRing is not advised. NuvaRing is available by prescription only.
Long-acting reversible contraception
Long-acting reversible contraception (LARC) are birth control options that last for several years and are reversible, meaning if you want to get pregnant or if you want to stop using them, you can have them removed at any time. LARC methods are highly reliable and are ideal for those who are concerned with an unplanned pregnancy yet want the flexibility to allow their body to have a quick turnaround to be fertile.
When using the LARC method, women tend not to have very light, and irregular menstrual periods, potentially with frequent cases of spotting. This can be frustrating for some, however, most of the time is easily corrected.
The Depo shot, brand name Depo-Provera®
Depo-Provera®, often called the “Depo shot,” is the branded name for medroxyprogesterone acetate, an injection that contains progestin and is given every three months. Typical use shows 94% effectiveness at preventing pregnancy The Depo shot prohibits the ovaries from releasing an egg and thickens the cervical mucus, keeping sperm from reaching the egg.
For many women, not having to remember to take birth control every day is a real benefit. In addition, Depo-Provera does not contain estrogen, a good option if you are not able to use products containing estrogen due to health problems. The Depo shot can decrease or stop menstruation, cramps, and pain. If you have risk factors for any of the following, your provider may advise against this form of birth control: vaginal bleeding, breast cancer, liver disease, osteoporosis, depression, heart attack or stroke.
Ongoing maintenance is required with Depo-Provera as you will need to schedule injection appointments with a nurse every three months. When you are ready to become pregnant, fertility may return immediately, but in some cases, may take over a year.
Birth control implant, brand name Nexplanon®
Nexplanon® is a small, thin, and flexible implant that is placed discreetly under the skin of the inner arm during an in-office procedure. The use of a numbing agent such as Lidocaine minimizes any discomfort. Nexplanon has been proven to be over 99% effective in preventing pregnancy by releasing progesterone to prevent ovulation while thickening the mucus around the cervix for up to three years.

Women have noticed menstrual changes, where menses may be lighter with less cramping, sometimes irregular, patchy or absent due to the hormones.
The implant can be removed at any time, and it is possible to become pregnant as early as a week after removal. If you do not want to get pregnant, you should start another birth control method right away.
Intrauterine Device (IUD): hormonal and copper coil
For those who don’t want the daily hassle of remembering to take their birth control, an intrauterine device (IUD) is a good option. An IUD is a small plastic T-shaped device inserted into the uterus where it blocks sperm from meeting the egg. IUDs are more than 99% effective in pregnancy protection. There are two types of IUDs, one contains a low dosage of hormones, and the other, which has a copper coil, does not. Hormonal IUDs can prevent pregnancy for up to 5 years, the copper for up to 10 years.
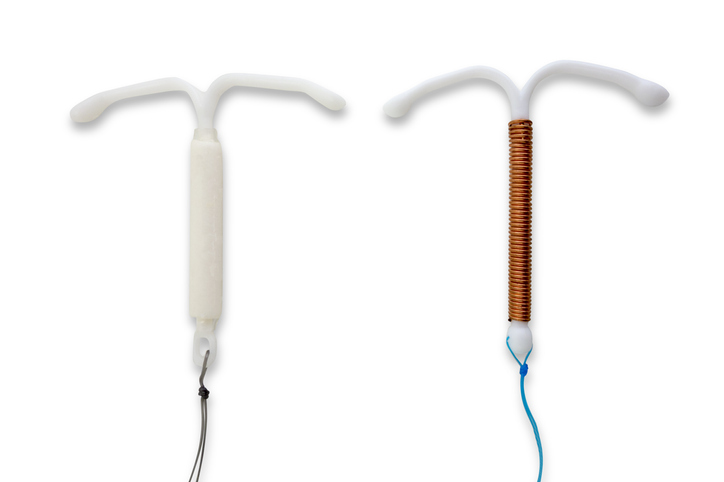
Both are very different, however, are fully effective against pregnancy when inserted.
Typical side effects include anemia, spotting, vaginal discharge, breast tenderness, headaches, nausea, weight gain, acne, and mood changes. Insertion can be painful and menstrual cycles unpredictable. Some women experience longer and/or heavier menstrual cycles, while others experience very light or minimal menses. An IUD can be removed at any time if fertility is desired or if the side effects are bothersome.
Common brand names for hormonal IUDs include Mirena®, Kyleena®, while Paragard®, remains a popular brand name for the copper coil type.
It should be noted that IUDs can be much more expensive than other types of birth control, but are usually covered by insurance.
Permanent birth control
Tubal ligation
When you have made the decision that you no longer want to become pregnant, two permanent birth control options are available: tubal ligation for women, and vasectomies for men. Both are effective at preventing pregnancy and are both very difficult, almost impossible, to reverse.
With tubal ligation, women undergo a surgical procedure in which their fallopian tubes are either tied, banded, sealed off, or removed altogether, preventing an egg from traveling into the uterus. Tubal ligation is an outpatient procedure with a short recovery. There are no known long-term side effects.
There is a very, very small chance of getting pregnant after the procedure, with percentages continually reducing as the number of years increase after the procedure. Studies show that less than 1% get pregnant after a tubal ligation.
Things to consider before a tubal ligation: the possibility of changing your mind and wanting a baby with a new partner or spouse, scarring, and complications, risks and costs associated with trying to reverse the procedure.
Vasectomy
A vasectomy is a simple and permanent procedure for men that is nearly 100% safe and effective. The vas deferens, the tubes that carry sperm, are either tied, cut and the ends cauterized or blocked with surgical clips. This procedure is less painful, invasive, and safer than a women’s tubal ligation where recovery tends to be a couple of days versus several weeks. Men must remember to check back in with their doctor to make sure their semen is free of sperm. Men, like women, need to consider the permanency of this procedure and the risks, costs and complications associated with a potential reversal.
Choosing the right birth control
Choosing the appropriate birth control option for you is an important decision you should consider with the guidance of your healthcare provider. With so many options, it’s important to discuss and consider which is best to meet your healthcare goals and support optimal health.
Make an appointment with Heidi Deutschlander, Women’s Health Nurse Practitioner or your family medicine provider in Mora, Hinckley or Pine City to discuss which birth control options are best for you. Call us at 800.245.5671 today or make an appointment online with MyChart.