As we age, like it or not, our bodies change. Some of these changes, like the gray hair and wrinkles, are obvious. Others are more subtle but perhaps even more important for us to understand.
Over time, changes in cells, tissues and entire organs eventually result in changes in function and appearance. While we cannot stop the march of time, there may be lifestyle changes that may slow progression.
Changes that come with age
Heart
- What changes? As with other muscles in the body, the heart muscle can weaken over time. For individuals who become less active as they age, the heart’s left ventricle stiffens and pumps less oxygen-rich blood to the body. The coronary arteries may experience a buildup of plaque called atherosclerosis which can reduce blood flow to the heart as they narrow and harden. High blood pressure can result and contribute to heart disease, heart failure (when the heart is no longer able to pump enough blood to meet the body’s needs) and heart attacks (when blood flow to the heart is suddenly blocked).
- What can I do about it? First, if you smoke, quit. Follow a healthy lifestyle based on regular physical activity and a heart-healthy diet with plenty of fruits and vegetables. Limit your intake of processed foods. Keep at a healthy weight. Have your blood pressure and cholesterol checked regularly. If you have or are at risk for diabetes, have your A1C checked periodically.
Bones, joints and muscles
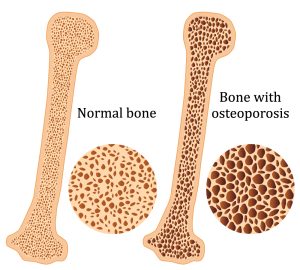
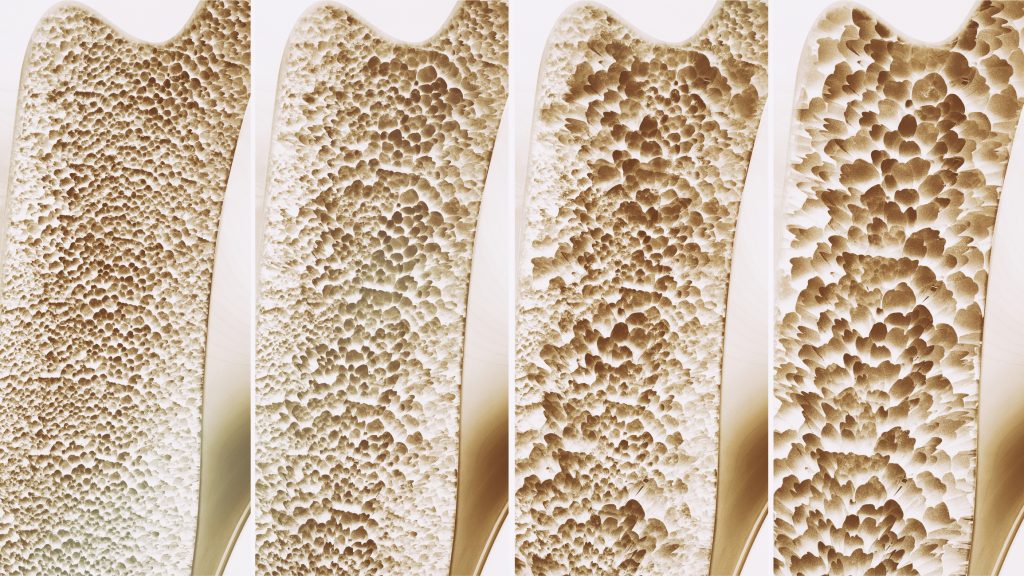
- What changes? Our bones lose density and become more fragile as the mineral content in our bones decreases. Loss of bone mass can lead to osteoporosis and bone fractures, often in the vertebrae or hips. In our joints, the cartilage that acts as a cushion begins to break down from years of repetitive motion leading to inflammation and arthritis. Joint motion becomes more restricted as tendons and ligaments begin to stiffen and lose elasticity. Our muscles start to shrink, with muscle mass declining as the number and size of muscle fibers decrease.
- What can I do about it? Stretching is an excellent way to help maintain joint flexibility. Weight training can increase muscle mass and strength, enabling people to continue their daily activities without maximal exertion. Long-term regular exercises may slow the loss of muscle mass and prevent age-associated increases in body fat.
Eyes
- What changes? As we age, the physical structure of our eyes changes. Eventually, this impacts our ability to focus on nearby objects, distinguish specific colors, or adjust to changing light levels. While these problems are often easily fixed with corrective lenses, other age-related conditions could be more concerning. These include age-related macular degeneration, diabetic retinopathy, cataracts, glaucoma, and dry eye.
- What can I do about it? Protect your eyes from sunlight by wearing sunglasses that block ultraviolet light. To prevent eye strain from sitting at a computer, take a break every 20 minutes to look about 20 feet away for 20 seconds. If you smoke, quit. Monitor your blood pressure.
Ears
- What changes? Hearing loss typically happens slowly over time. An estimated 3 in 10 adults over 65 have some age-related hearing loss or presbycusis. Changes to the inner ear, middle ear, or nerves are most often to blame. In addition to age, other variables that may impact hearing include diabetes, ear infections, blood pressure, medications, exposure to loud sounds, and heredity.
- What can I do about it? Preventing age-related hearing loss includes measures used to prevent noise-induced hearing loss. Be careful to avoid loud noises, reduce the amount of time exposed to loud noise, and protect your ears with ear plugs. If hearing loss has already occurred, you may wish to consider hearing aids.
Skin
- What changes? For many, the first age-related changes to our skin are rough, dry patches that can feel scaly or itchy. Most, at some point, will notice their first wrinkles, inevitable as the skin becomes thinner, loses fat, and no longer appears plump and smooth. Years of sun exposure and habits such as smoking can quicken this process. As skin thins, it becomes more transparent and more fragile. It takes longer to heal from cuts and scratches, and bruises. Age spots and skin tags are common in older individuals but harmless. A more significant concern is skin cancer. Most skin cancers are caused by the sun and are generally curable if caught before spreading.
- What can I do about it? Limit your time in the sun. Seek shade whenever possible. Wear a broad-spectrum sunscreen with an SPF of 15 or higher when outside. Wear a wide-brim hat and cover up with sun-protective clothes. Consider a self-tanner rather than be exposed to UV rays. Wear sunglasses to limit squinting. If you smoke, stop. Limit alcohol which dehydrates the skin. Be gentle when cleaning. Moisturize your skin daily.
Teeth and gums
- What changes? Our teeth put up with a lot of wear and tear. Over the decades, the protective coating of enamel on the teeth can wear away, leading to tooth discoloration, cracks and breaks and an increased chance of infection. Dental decay can also result from dry mouth, common among older adults, decreased saliva production, and a side effect of many common medications. The chance of severe tooth damage, enough to require a root canal, triples at age 65. Gum problems, including receding gums and gum disease, are common in older adults and, if undiagnosed and untreated, can lead to irritation, inflammation or even loss of teeth.
- What can I do about it? Cut down on wear and tear by avoiding chewing on ice or hard foods. If you grind your teeth, consider wearing a night guard when you sleep. Keep your gums healthy with regular brushing and flossing. If you smoke, quit. Drink tap water containing fluoride to help prevent tooth decay.
Aging cannot be avoided, but it can be done gracefully. To start, be proactive with your health and your healthcare by scheduling annual exams and talking to your provider when you have questions. Don’t put off asking about your concerns. Your Welia Health provider is here for you.